“It’s not possible for women with breast implants to breastfeed.”
Wrong! Not only can women with implants breastfeed, but they can also do it without any concerns regarding the safety or quality of milk.
If you’ve been considering breast surgery but have hesitated in order to start a family, let us help you clear up some misconceptions, so you can navigate modern motherhood on your terms!
Breastfeeding and How Your Breasts Actually Work
With more and more women in the UK opting for breast augmentation , and also showing a preference for breastfeeding over bottle feeding this becomes an important topic for discussion.
As you explore breastfeeding and the impact of breast augmentation surgery on it, it might help to start by learning more about your breasts’ anatomy. Under your skin, different structures make up each of your breasts.
When feeding milk to an infant, ducts carry milk from the lobules to the surface of your nipple. The prolactin hormone promotes the production of milk in the breasts (also known as lactation) when you’re pregnant.
Another hormone – oxytocin (also known as the ‘milk ejection reflex’), helps in the release and flow of milk from the lobules to the nipples. Both the prolactin and oxytocin hormones work together to build milk supply and the tissues ensure you’re able to breastfeed. Oxytocin also helps you bond with your infant which is especially helpful during the early days as both you and your baby learn how to breastfeed.
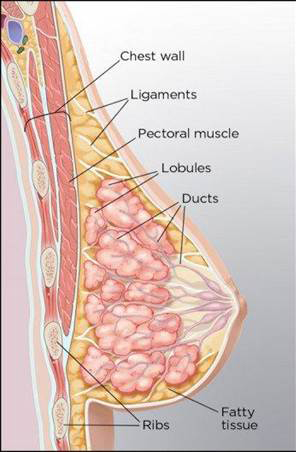
Chest Wall: The chest wall includes bones, skin, tissues, and muscles that protect all your internal organs between your neck and abdomen.
Pectoral Muscles: The pectoral muscles provide support to your breasts, help stabilise your shoulder joints, and strengthening them improves your breathing.
Lobules: Lobules are glandular tissue responsible for producing milk. They are found in the fatty tissue layer, in clusters called lobes around the nipple.
Ducts: Ducts connect the lobules to form a complex network that carries milk to the nipple when the baby suckles.
Fatty Tissue: Fatty tissues occupy the space between your lobes and ducts and fibrous tissue (ligaments) and hold the structure of your breast together.
Lymph Nodes: These small organs (also present in other regions of your body) produce lymphocytes or white blood cells to protect your body against disease and infection.
Types of Breast Surgery and How It Affects Breasts
Now that we’ve understood the anatomy and functions of the different structures in a breast, how do your breasts change when you get breast implants and what does it mean for you if you want to breastfeed?
There are two types of breast augmentation procedures: augmentation with breast implants and fat transfer augmentation. During fat transfer breast augmentation, liposuction techniques are used to remove fat from inner thighs, stomach, or back and safely transfer into your breasts via small incisions whose location aren’t likely to impact milk expression. With breast implants, however, the type of incision and location are critical as they may pose some challenges to milk supply.
Breast Implant Incision Methods and Nursing
There are three common breast augmentation incisions used to insert implants, each suited to different aesthetic and lifestyle outcomes.
Inframammary Incision (Under the Breast): The most popular breast augmentation incision technique, made under the breast crease.
Periareolar Incision (Around the Nipple): Incision is made between the areola and the skin surrounding the breast.
Transaxillary Incision (Under the Armpit): This involves creating a careful incision in the armpit’s natural fold.
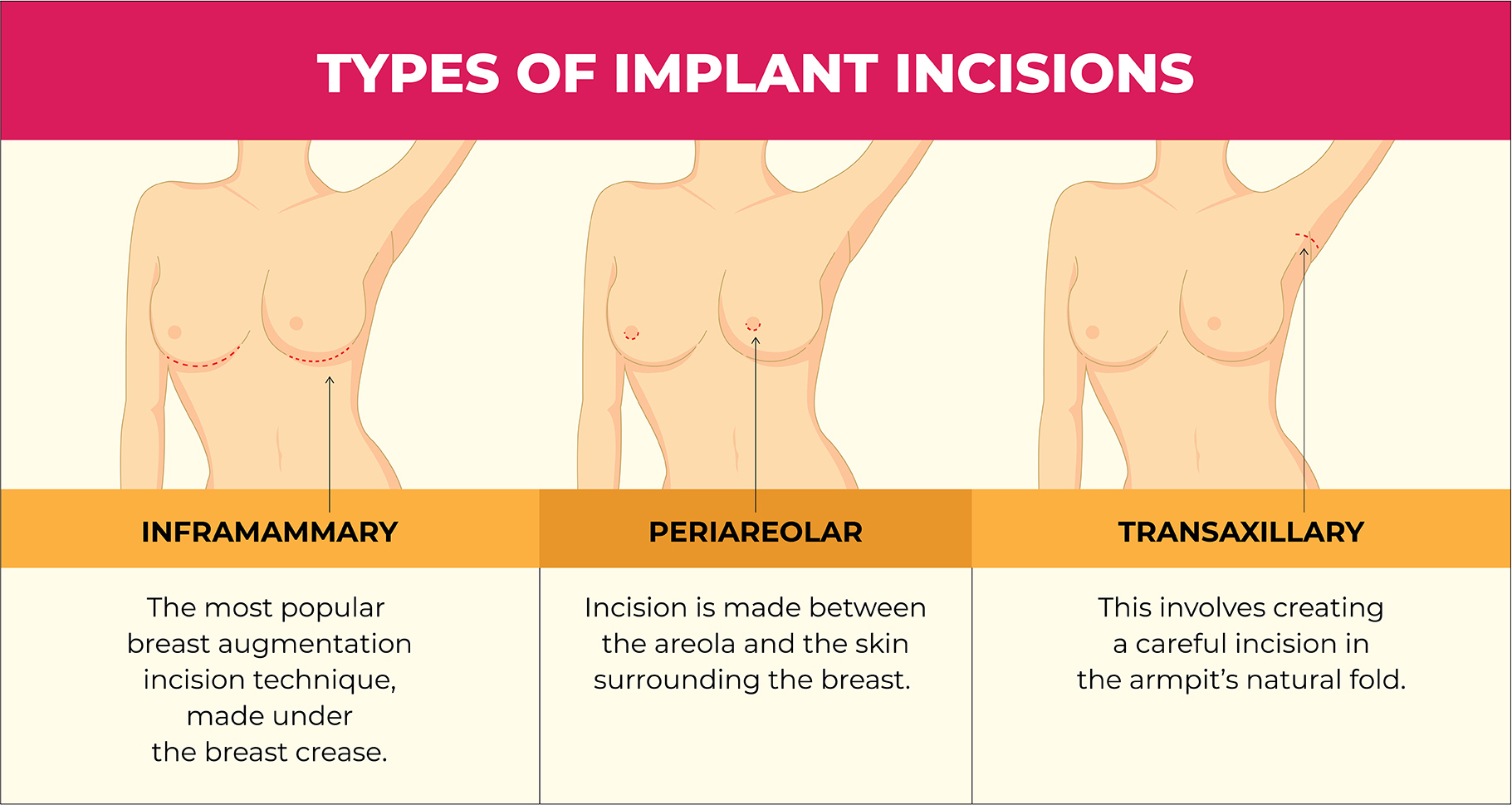
When it comes to nursing success, nipple sensation has a crucial role to play. This is because sensation from suckling stimulates a woman’s pituitary gland to release prolactin and oxytocin hormones, which in turn enables milk production and release. With any incision approach, it is therefore critical to preserve the neural pathways.
There’s no evidence that suggests an incision type is superior. Neither do incisions made around your armpit or under the breast crease pose a significant challenge to milk expression. However, the periareolar incision was five times more likely to be associated with insufficient milk supply than no surgery, as it presents a higher chance of damaging one of these nerve branches – the lateral intercostal branch of T4, that passes through its route.
Why Breast Implant Placement Techniques Matter for Breastfeeding
Having made the incision, there are three placement techniques that are predominantly used in a breast augmentation surgery.
Subglandular (Behind the breast) – The simplest of breast augmentation procedures, it involves placing the breast implant behind the breast tissue.
Submuscular (Behind the muscle) – In this method, the implant is placed behind the breast muscle to provide more coverage to it and in case there’s very little breast tissue.
Dual plane augmentation – This method is a combination of the previous two techniques and involves placing the implant partly behind the breast tissue and partly behind the breast muscle.
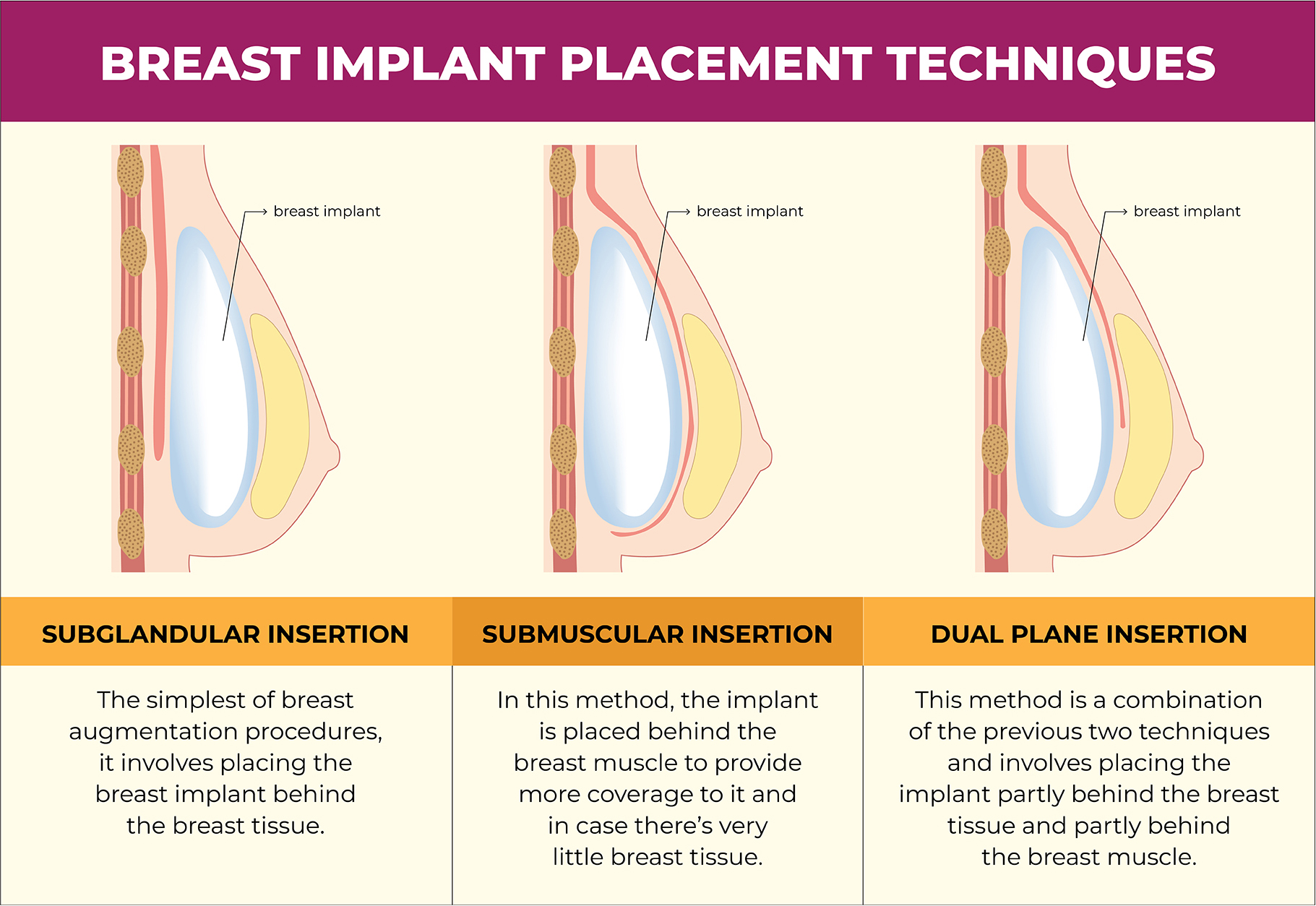
Since the implants are placed under the breast tissue, the muscle, or between the two, there’s little to no interference with the ducts that carry the milk to the nipples or the glands for milk production.
Still, women with implants placed under the breast were found to be less able to breastfeed versus women with implants placed under the muscle. This is because breast implants placed under the breast tissue can compress the milk ducts and nerves responsible for carrying milk to the nipple.
What Other Factors Contribute to Breastfeeding Challenges
Reduced lactation capacity may also result from surgery-related complications such as capsular contracture, infection, or pain that can make breastfeeding difficult.
While multiple studies have indicated that breast implants pose no significant challenges to nursing, a comparative review of three studies suggests that breast augmentation surgery is associated with 40% decrease in exclusive breastfeeding, and bigger implants [270 ml or more] and saline implants may contribute to inadequate milk supply.
Despite these challenges, new mothers with breast augmentation are reported to have 75% chance of breastfeeding, if they wanted. If the implants are placed behind the muscle, their chances increase to 82%.
We recommend discussing all your options with your surgeon or healthcare provider during your pre-operative consultation and settling on the procedure that best suits your aesthetic and life goals, especially if it includes breastfeeding in the future.
Debunking Myths about Breastfeeding with Breast Implants
Babies refuse milk from breasts with implants.
False! Babies’ willingness to breastfeed depends on milk supply and latching comfort, not on whether or not you’ve had breast implant surgery.
Breast implants change the composition of breast milk.
Breast implants do not alter or impact the composition or taste of breast milk. Neither does having implants imply that your breast milk could end up having excessive silicone or saline (both of which are naturally found in the human body and in breast milk at safe levels).
Silicone from the breast implant can leak into the breast milk.
Untrue! Research shows that silicone molecules are too large to leak into breast tissues or the milk ducts, and therefore, poses no risk to nursing infants. Studies also indicate that breastfeeding moms with silicone implants had the same levels of silicone in their breast milk as moms without implants.
Silicone implants are not safe for nursing moms.
Both saline and silicone implants are safe. Silicone used in breast implants is medical-grade, extensively tested, and can’t contaminate breast milk.
Risk of mastitis increases with breast implants.
Wrong! Mastitis is a bacterial infection that presents flu-like symptoms. It is not caused by breast implants. On the contrary, bad hygiene, poor milk expression technique, or cracked nipples may have a role to play.
Breastfeeding will rupture breast implants.
Breast implant rupture is very rare. Considering how they’re placed and protected, your baby can’t damage them when nursing.
Staying Abreast of Restrictions and Activities
In the first few weeks after your breast surgery, your focus should be on rest and limited movement. Light activities like short walks are encouraged to help with your blood circulation, but avoid any movements that strain the chest or upper body.
Always pay close attention to your body and do not try to push beyond your comfort level.
Returning to Work: Your return to work will depend on the nature of your job. For desk jobs, you may return within 2-3 weeks, but more physically demanding roles might require 4-6 weeks off. Talk to your supervisors to help gradually ease back into your routine, and avoid tasks that could strain your chest or incisions.
Carrying Young Children: Avoid lifting or carrying young children for at least 4-6 weeks post-surgery. If you need to hold them, ask someone to place the child on your lap while seated. Explain to your children that mummy needs time to heal, and seek help from family or friends for childcare duties.
Housework and Chores: Limit cooking and cleaning for the first few weeks. If necessary, only perform light tasks that don’t require bending, lifting, or stretching. Do think ahead about how to manage meals and any daily routines you may have. Avoid vacuuming, mopping, or any activity that involves upper body strain until you’re fully cleared by your surgeon.
Getting Around: After breast surgery, it’s crucial to avoid driving until you’ve recovered and received medical clearance. Initially, you might experience limited mobility and discomfort, which can affect your ability to drive safely. Arrange for ridesharing services or taxis to get around safely. Alternatively, ask family and friends for help with lifts and errands.
Activities and Lifting: Avoid lifting any weights for the first two weeks after your surgery. Even after that, refrain from lifting anything heavier than half a kg, including children or groceries. Avoid strenuous activities like bending, stretching, or exercising, as these can strain the surgical site and impede healing. Even seemingly simple tasks, like reaching overhead, should be avoided until cleared by your surgeon.
| WEEKS | ACTIVITIES | DETAILS |
1-2 | Rest and Light Activities | Concentrate on getting some rest. Steer clear of labour-intensive tasks, vigorous exercise, and heavy lifting. If at ease, light walking is recommended. |
3-4 | Light Chores and Gentle Exercise | Return to simple home chores gradually. Begin mild physical activities, such as gentle stretches or quick strolls. |
5-6 | Moderate Work and Exercise | Restart some planned exercises and mild work tasks. Steer clear of intense exercise or heavy lifting. |
7-8 | Increased Workload and Exercise | It’s time to now begin your work-related activities, and up the tempo of your workouts. Remember to run any high-impact activities by your surgeon first. |
9-12 | Full Activity Resumption | No complications? Then you are ready to step back into your routine! |
Common Issues Breastfeeding Mothers Face
Without breast augmentation too, factors such as sore nipples, breast engorgement, blocked ducts, infection, latching difficulties, lactation inhibition, or pre-existing health conditions may contribute to a reduced milk supply and milk expressing difficulties. In fact, some of the most common problems new moms may face have little to do with their implants and are reported among mothers without implants as well.
Breast Hypoplasia: Some women may report having underdeveloped breast (or glandular) tissue before undergoing breast augmentation surgery. This condition is called breast or mammary hypoplasia and presents in the form of tubular breasts that are significantly asymmetrical and placed wide apart. It’s important to note that mothers with this condition may not be able to produce enough milk and are advised to seek prenatal and postpartum support to ensure your newborn receives nutrition for growth.
Inadequate Milk Production & Supply: If the breast implants impede milk production structures, they may result in a decreased supply. At times, the size and placement of implants can also put pressure on the glandular tissues and interrupt milk production and supply.
Breast Engorgement: Engorgement is when your breasts get too full with milk and typically happen in the early days when your baby is still getting used to breastfeeding. This may be expected in mothers with and without breast implants. However, with an implant, it may be more uncomfortable for you.
Mastitis: An infection in the breasts, mastitis can be painful and presents flu-like symptoms. It affects 1 in 10 women and causes the breasts to become red, swell, and experience a burning sensation when nursing. Mastitis may lead to capsular contracture if not treated in time, which causes painful scarring around the breast implants and hardening of breasts.
Tips for Breastfeeding Success
- Develop a Breastfeeding Routine – A consistent and frequent feeding routine may be beneficial for both your baby and you. It’ll send your body the right signals to improve milk production and expression. Adhere to the routine and avoid skipping feedings.
- Empty the Breasts during Feeding – Try to empty both breasts during each session to signal your body to produce more milk. Offer both breasts during the feed and switch breasts mid-way.
- Watch Your Hydration & Nutrition – Taking care of yourself is critical for optimal milk production. Ensure you’re on a balanced diet rich in nutrients important to lactation, properly hydrated, and that you eat often.
- Try Skin-to-Skin – During feeding sessions, skin contact stimulates milk production. If uncomfortable (it sometimes can be when you have breast implants) seek professional advice.
- Consult a midwife – Before starting your journey, consult a professional to ensure you and your baby have a healthy, nourishing, and beautiful bond.
Note: Please inform your GP or healthcare provider if you’ve undergone breast surgery before conceiving so that they can effectively guide you on your breastfeeding journey and manage issues that may emerge.
Questions about Breastfeeding with Breast Implants Answered
Is nursing painful with implants?
There may be excessive sensitivity in your breasts and nipples because of your breast implants, but breastfeeding shouldn’t be painful. Consult your surgeon or GP if it is.
Will breastfeeding undo the results of my breast augmentation?
Breastfeeding doesn’t change the size of your implants! Some change in the shape of your breasts is to be expected though, because of changes to your breast tissues due to pregnancy and lactation.
Can I exclusively breastfeed my baby?
You may or may not be able to exclusively breastfeed. This depends more on milk production and its supply to your nipples and less on your implants. It’s best to monitor your baby’s weight gain in the early weeks to ensure they’re getting adequate nourishment.
Which method of implant placement is best for breastfeeding my baby?
Placement of breast implants is personalised in consultation with your surgeon and in accordance with your needs and goals. It’s best to consult your surgeon about it before the breast augmentation and outline your goals including your intention to breastfeed.
If it’s not my breast implants that’s preventing me from breastfeeding, what is it?
It’s possible an underlying medical reason such as PCOS, Hypothyroidism, Breast Hypoplasia, or Capsular Contracture is preventing you from nursing your baby. Consult with your GP for a holistic evaluation.
Conclusion
The UK reportedly has some of the lowest breastfeeding rates in the world, with only 34% of mums nursing at six months and 0.5% at 12 months. Improving these rates can greatly benefit your child’s health, and having breast implants in no way prevents or hinders your from nursing your baby .
Being a parent and learning to care for your newborn can be intimidating, and for new mothers, successful nursing comes with practice and patience. If you’ve undergone breast augmentation prior to your pregnancy, you might need to be a little more careful so as to care for your implants as you care for your baby.
A good and personalised pre-operative consultation that outlines the process of breast augmentation is likely to put you more at ease as well as contribute to your breastfeeding success when you’re at that point of your life.
You may also enlist help from your spouse, partner, family, and friends to help you breastfeed. If you’re able to or need to, consult a newborn care specialist to show you the tricks to essential and effective care that doesn’t put your breast implants at risk.
***
Footnotes
Institute of Medicine (US) Committee on the Safety of Silicone Breast Implants; Bondurant S, Ernster V, Herdman R, editors. Safety of Silicone Breast Implants. Washington (DC): National Academies Press (US); 1999. 11, Effects On Pregnancy, Lactation, and Children.
Kazankaya F, Ahsun Paker S, Demirel Bozkurt Ö. Breastfeeding After Breast Augmentation Surgery: A Scoping Review. Florence Nightingale J Nurs. 2024 Feb 1;32(1):99–109. doi: 10.5152/FNJN.2024.23231. PMCID: PMC11059175.
Schiff M, Algert CS, Ampt A, Sywak MS, Roberts CL. The impact of cosmetic breast implants on breastfeeding: a systematic review and meta-analysis. Int Breastfeed J. 2014 Oct 17;9:17. doi: 10.1186/1746-4358-9-17. PMID: 25332722; PMCID: PMC4203468.
Bompy L, Gerenton B, Cristofari S, Stivala A, Moris V, See LA, Rizzi P, Braye F, Meningaud JP, Zwetyenga N, Guillier D. Impact on Breastfeeding According to Implant Features in Breast Augmentation: A Multicentric Retrospective Study. Ann Plast Surg. 2019 Jan;82(1):11-14. doi: 10.1097/SAP.0000000000001651. PMID: 30325833.
Scime NV, Metcalfe A, Nettel-Aguirre A, Nerenberg K, Seow CH, Tough SC, Chaput KH. Breastfeeding difficulties in the first 6 weeks postpartum among mothers with chronic conditions: a latent class analysis. BMC Pregnancy Childbirth. 2023 Feb 2;23(1):90. doi: 10.1186/s12884-023-05407-w. PMID: 36732799; PMCID: PMC9893695.
Jewell ML, Edwards MC, Murphy DK, Schumacher A. Lactation Outcomes in More Than 3500 Women Following Primary Augmentation: 5-Year Data From the Breast Implant Follow-Up Study. Aesthet Surg J. 2019 Jul 12;39(8):875-883. doi: 10.1093/asj/sjy221. PMID: 30165661; PMCID: PMC6624791.